- Have any questions?
- +91-98717 17305
- babiesandus12@gmail.com
Period After 2 Years Menopause: Causes, Risks & Medical Actions

Heavy Period at Age 53: Understanding Menstrual Shifts in Midlife
November 14, 2023Navigating Being Pregnant at 44
December 15, 2023Getting vaginal bleeding after two years without a period? It’s definitely unsettling, and honestly, it’s not something to brush off. Any vaginal bleeding two years post-menopause isn’t considered normal and really does need a doctor’s input, pronto. Menopause is officially in the books after 12 months straight with no period, and if you start bleeding again after that, it’s not just your cycle making a comeback.
This can feel scary, which is exactly why we put this together—to give you some clarity about what’s going on. Postmenopausal bleeding can have a bunch of causes, ranging from harmless to, well, less so. Either way, seeing a healthcare provider is the only way to get answers and a bit of peace of mind.
We’ll break down why bleeding after menopause is a big deal, what might be causing it (from vaginal dryness to more serious stuff), and what usually happens at the doctor’s office. The idea is to give you straightforward info so you can make the best decisions for your health—without getting overwhelmed by medical jargon.
Why Bleeding Two Years After Menopause Matters

Any bleeding after menopause isn’t something to ignore. It’s your body’s way of waving a red flag, even if the bleeding is just a little bit or looks like a full-blown period. Bleeding after menopause should always be checked out, no matter the amount.
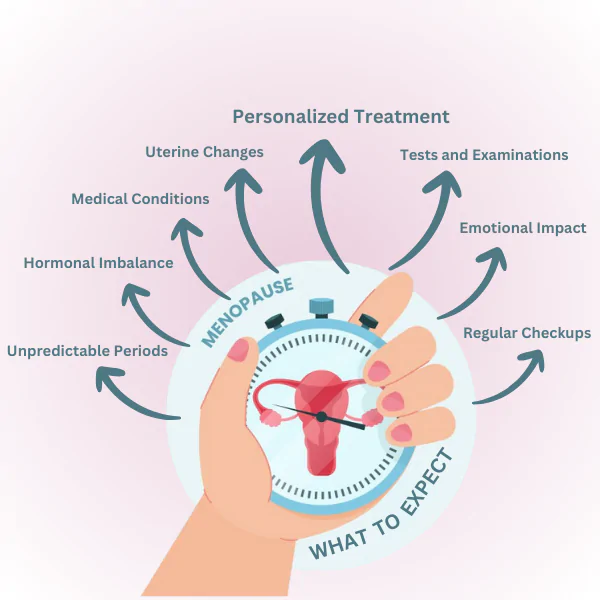
Understanding the Definition of Menopause and Postmenopause
Menopause is marked by 12 months in a row with no period. Most folks hit this between 45 and 55, with the average being around 51. After that year, you’re officially in postmenopause.
In postmenopause, your ovaries are pretty much done making oestrogen and progesterone, so ovulation and periods stop for good.
Two years out with no periods? That’s postmenopause, fully settled in. Periods don’t just pick up again at this point—the hormones just aren’t there to make it happen. So, any new bleeding isn’t a “normal” period; it’s a sign something else is up.
It’s easy to assume a random bleed just means your cycle is back, but that’s not really how it works. And thinking that way can actually delay getting the help you might need.
Differentiating Between Spotting and Period-Like Bleeding
Spotting is that light, barely-there bleeding—maybe just a smudge on the toilet paper, or enough for a panty liner. Period-like bleeding is heavier, more like what you remember from before menopause, and might need pads or tampons.
But here’s the thing, whether it’s spotting or a heavier flow, both are reasons to check in with your doctor. The amount doesn’t really tell you how serious it is, unfortunately.
Some women get one episode of light spotting; others have repeated bleeding. It could be bright red, pinkish, brown, or mixed with discharge. Sometimes it’s after sex or exercise, sometimes it just shows up out of nowhere.
Some patterns you might notice:
- Just one little spot of blood
- Light pink or brown discharge that hangs around for a few days
- Bleeding that feels like a light period
- Heavier bleeding, maybe with clots
- Bleeding after sex
We can’t say it enough: postmenopausal bleeding needs checking out, no matter how much or how often. You just can’t tell what’s causing it based on the amount or look of the blood.
Immediate Risks and Red Flags
About 1 in 10 women with bleeding after menopause actually have uterine cancer. That’s why doctors take it so seriously right from the start.
Endometrial cancer is the main worry. Most women with this cancer notice abnormal bleeding as their first tip-off. Catching it early really does improve the odds, so don’t put off making that appointment.
There’s also endometrial hyperplasia, which is a fancy way of saying the lining of your uterus is growing in an abnormal way. It’s not cancer, but it can turn into cancer if left untreated. So, it’s not something to ignore either.
Call your doctor ASAP if you notice:
- Any vaginal bleeding after two years period-free
- Bleeding that comes with pelvic pain or pressure
- Bleeding with a bad-smelling discharge
- Bleeding after sex
- Bleeding along with unexplained weight loss
Seriously, don’t wait to see if it just goes away. Any bleeding after menopause needs a quick check—think days, not weeks. Yes, sometimes it’s something simple like dryness or a polyp, but only a medical exam can say for sure.
Potential Causes, Evaluation, and Management of Postmenopausal Bleeding
Bleeding after menopause isn’t something to put off—it’s important to figure out what’s behind it. Causes range from totally harmless tissue changes to more worrying issues like cancer. The usual process? A good exam, maybe a few tests, and then treatment that fits whatever’s actually going on.
Most Common Causes of Bleeding After Menopause
Most postmenopausal bleeding cases are actually benign. The top reasons are endometrial atrophy (thinning of the uterine lining) and vaginal atrophy (the same thing, but in the vagina). Both happen when oestrogen drops off, making tissues fragile and prone to bleeding.
Polyps—those little growths on the uterus or cervix—are also common. They’re usually harmless but can bleed, especially after sex or exercise.
Endometrial hyperplasia is another culprit. That’s when the uterine lining thickens up, often because of too much oestrogen and not enough progesterone. Sometimes it’s just an odd growth, sometimes it’s a warning sign.
Other less-worrisome causes can include:
- Uterine fibroids that linger after menopause
- Atrophic vaginitis (dry, inflamed vaginal tissue)
- Cervicitis or endometritis from an infection
- Hormone therapy that stimulates the uterine lining
Diagnostic Examinations and Tests
First step is usually a pelvic exam. The doctor checks for anything obvious—polyps, lesions, irritation—that could be causing the bleeding. They want to see exactly where the blood’s coming from.
Then comes a transvaginal ultrasound, which is a pretty standard way to measure how thick the uterine lining is. If it’s under 4-5 millimetres, that’s usually reassuring. If it’s thicker, more digging is needed.
Endometrial biopsy is still the gold standard if the ultrasound looks suspicious or just doesn’t answer the question. It’s a quick office procedure—just a tiny sample of the uterine lining to look at under a microscope.
Other possible tests:
Test | Purpose |
Hysteroscopy | Lets the doctor see inside the uterus directly |
Sonohysterography | Uses saline and ultrasound to spot polyps or growths |
Cervical cytology | Checks for abnormal cells on the cervix |
Dilation and curettage | Samples more of the uterine lining for a thorough look |
Endometrial cancer is the biggest concern, showing up in about 10% of women with postmenopausal bleeding. For most, the first clue is abnormal vaginal bleeding—so catching it early really matters.
Cervical cancer is another, though less likely than endometrial cancer at this age. Regular Pap smears are still important for picking up any early changes.
Endometrial hyperplasia with atypia is a mouthful, but it means there are abnormal cells in the uterine lining that could turn into cancer. It needs close follow-up and sometimes more aggressive treatment.
Things that raise your risk for these cancers include:
- Obesity and metabolic syndrome
- Long-term unopposed oestrogen (without progesterone to balance it)
- Tamoxifen therapy
- Lynch syndrome or a family history of uterine/colon cancer
- Diabetes
Treatment and Follow-Up Care
Treatment really hinges on what’s found during evaluation. Atrophic conditions? Those usually do well with local oestrogen therapy—applied vaginally—which tends to restore tissue health without much risk of it spreading systemically. It’s a straightforward fix for a common problem.
Polyps are removed via hysteroscopic polypectomy, which is minimally invasive and gets the job done while letting us examine the tissue properly afterward. Most people notice their symptoms clear up after this, though there’s always a small chance of recurrence down the line.
For endometrial hyperplasia without atypia, progestin therapy is often enough to reverse things. If atypia is present, though, hysterectomy is usually advised because of the cancer risk. We keep an eye on how things are going with repeat endometrial sampling, just to be sure the treatment’s working.
When it comes to malignancies, patients need a referral to gynaecological oncology for proper surgical staging and figuring out the next steps. Early-stage endometrial cancer, if it’s still just in the uterus, generally responds well to timely intervention—so catching it early matters.
Follow-up care means watching for any bleeding that comes back and reassessing if symptoms pop up again. Women who’ve had conservative treatment need regular check-ins to make sure everything’s resolved, while those with risk factors might need closer, ongoing surveillance. It’s not always a one-and-done situation.
Conclusion

Experiencing bleeding two years after menopause might catch you off guard. However, it’s a reminder that our bodies can sometimes follow their own rhythm. While it’s not always cause for alarm, it should prompt us to stay attuned to our bodies and prioritize our health. Don’t hesitate to consult a healthcare professional if you encounter such an occurrence.
Navigating menopause is a unique journey for every individual. With medical guidance and support, you can confidently embrace the next phase of your life, ensuring your well-being remains a priority. Stay informed, empowered, and open to seeking assistance whenever needed.
Whether it is seeking treatment for post-menopausal bleeding or female infertility treatment in Mumbai, remember, we are here to help.
Contact us to schedule an appointment with our gynecological experts and IVF specialists in Mumbai at Babies & Us Fertility Center for expert guidance and personalized care.
FAQs
Q1. Is any bleeding after menopause normal?
No bleeding that occurs after menopause should be evaluated by a healthcare professional. While it might have benign causes, it’s essential to rule out more severe conditions.
Q2. What are some common benign causes of post-menopausal bleeding?
Non-cancerous conditions like uterine or cervical polyps, hormonal fluctuations, or thinning of the vaginal lining (atrophic vaginitis) can contribute to post-menopausal bleeding.
Q3. Could post-menopausal bleeding indicate a severe medical condition?Q3. Could post-menopausal bleeding indicate a severe medical condition?
It’s important to rule out serious conditions like endometrial hyperplasia or even endometrial cancer. Consult a doctor promptly if you experience any bleeding after menopause.
Q4. When should I seek medical attention for post-menopausal bleeding?
If you experience bleeding after two years of menopause, or if the bleeding is heavy, recurrent, accompanied by pain, or lasts more than a few days, consult a healthcare professional. It’s always better to have any unusual bleeding investigated by a doctor to ensure your health and well-being.