- Have any questions?
- +91-98717 17305
- babiesandus12@gmail.com
Period After 2 Years of Menopause: Causes, Risks & Medical Actions

Fundal Fibroid and Pregnancy
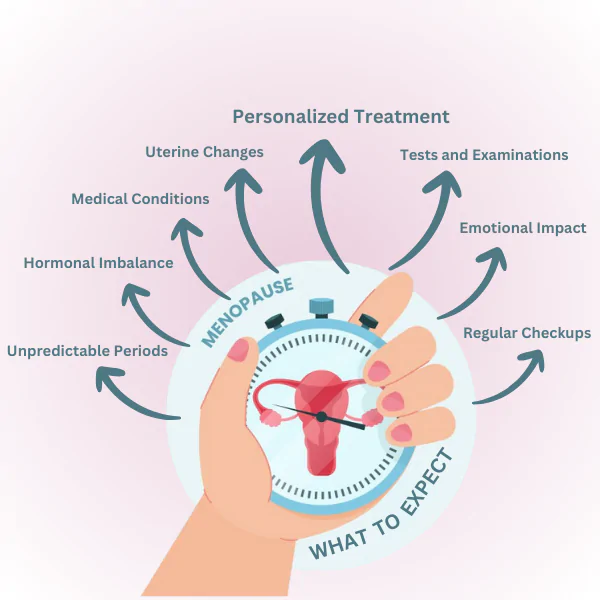
October 14, 2025Experiencing (vaginal bleeding) Period After 2 Years of Menopause can be a big scare and should be dealt with caution. Once menopause is declared—which is the case after a full year without period any later occurrence of vaginal bleeding is treated as abnormal and medical help is sought immediately. Hormonal activity responsible for menstrual bleeding has stopped, so this bleeding does not signal a comeback of the menstrual cycle.
This case may surely lead to stress and that is the reason why this guide is meant to be a source of clear and trustworthy information. Postmenopausal bleeding (bleeding after menopause) can have different origins, starting from the simplest one and ending with the most critical one. But still, it is the doctor’s verdict to rule out the cause and provide the right treatment that a gynecologist will be the one to consult. We will be discussing the importance of the bleeding after menopause, indicating possible reasons, telling what to expect during the medical evaluation, and suggesting the treatment options in this article. Our intention is to give you access to very precise information without letting you feel the burden of the complicated medical matter.
Why Period After 2 Years of Menopause Matters

Any vaginal bleeding after menopause is abnormal and should be promptly investigated. Whether the bleeding is light spotting or resembles a menstrual period, it is a clinical warning sign that warrants attention.
Understanding the Definition of Menopause and Post menopause
Menopause is diagnosed after 12 consecutive months without a menstrual period, typically occurring between the ages of 45 and 55, with the average age around 51. Following this transition, a woman enters post menopause.
During post menopause, the ovaries significantly reduce production of estrogen and progesterone. As a result, ovulation and menstrual periods permanently stop. Two years without periods confirms established post menopause, and menstrual bleeding does not resume naturally at this stage. Therefore, any vaginal bleeding occurring after this period is not a normal cycle and indicates an underlying condition that requires evaluation. Assuming it is a return of menstruation may delay necessary medical care.
Differentiating Between Spotting and Period-Like Bleeding
Spotting refers to minimal bleeding, such as light staining on toilet paper or underwear. Period-like bleeding is heavier and may require sanitary pads or tampons.
Importantly, the volume or appearance of bleeding does not indicate its seriousness. Even minimal spotting can be associated with significant medical conditions.
Postmenopausal bleeding may appear as:
- A single episode of light spotting
- Pink or brown discharge lasting several days
- Bleeding similar to a light menstrual period
- Heavier bleeding with or without clots
- Bleeding after sexual intercourse
Regardless of frequency or severity, all postmenopausal bleeding requires medical assessment.
Some patterns you might notice:
- Just one little spot of blood
- Light pink or brown discharge that hangs around for a few days
- Bleeding that feels like a light period
- Heavier bleeding, maybe with clots
- Bleeding after sex
We can’t say it enough: postmenopausal bleeding needs checking out, no matter how much or how often. You just can’t tell what’s causing it based on the amount or look of the blood.
Immediate Risks and Red Flags
Approximately 10% of women with postmenopausal bleeding are diagnosed with endometrial (uterine) cancer. This is why healthcare providers treat such symptoms with urgency.
Abnormal vaginal bleeding is often the earliest sign of Endometrial cancer. Early diagnosis significantly improves treatment outcomes. Another important condition is endometrial hyperplasia—abnormal thickening of the uterine lining—which is not cancer but can progress to malignancy if untreated.
Seek immediate medical attention if you experience:
- Any vaginal bleeding after two years without periods
- Bleeding accompanied by pelvic pain or pressure
- Foul-smelling vaginal discharge
- Bleeding after sexual intercourse
- Bleeding with unexplained weight loss
Do not wait to see if the bleeding resolves on its own. Timely evaluation within days rather than weeks is essential.
Causes, Evaluation, and Management of Postmenopausal Bleeding
Identifying the cause of postmenopausal bleeding is critical. While many causes are benign, some require urgent treatment. Evaluation typically involves a clinical examination, imaging, and, if needed, tissue sampling.
Common Causes of Postmenopausal Bleeding
The majority of cases are due to benign conditions. The most common include:
- Endometrial atrophy: Thinning of the uterine lining
- Vaginal atrophy: Fragile vaginal tissue due to low estrogen
Both conditions result from estrogen deficiency and can lead to tissue irritation and bleeding.
Other common causes include:
- Uterine or cervical polyps
- Endometrial hyperplasia
- Persistent fibroids
- Atrophic vaginitis
- Infections such as cervicitis or endometritis
- Hormone replacement therapy
Diagnostic Tests and Evaluation
Evaluation usually begins with a pelvic examination to identify visible sources of bleeding.
A transvaginal ultrasound is commonly performed to assess endometrial thickness. A lining thinner than 4–5 mm is generally reassuring. Thicker measurements require further investigation.
An endometrial biopsy is the definitive test when ultrasound findings are abnormal or inconclusive. This brief outpatient procedure allows microscopic examination of uterine tissue.
Additional tests may include:
| Test | Purpose |
| Hysteroscopy | Direct visualization of the uterine cavity |
| Sonohysterography | Detects polyps or structural abnormalities |
| Cervical cytology | Screens for cervical abnormalities |
| Dilation and curettage (D&C) | Comprehensive tissue sampling |
Serious Conditions Linked to Postmenopausal Bleeding
Endometrial cancer is the most serious concern and accounts for approximately 10% of cases. Early detection significantly improves prognosis.
Other conditions include:
- Cervical cancer
- Endometrial hyperplasia with atypia
Risk factors include:
- Obesity
- Diabetes
- Long-term unopposed estrogen exposure
- Tamoxifen therapy
Lynch syndrome or family history of gynecologic cancers
Treatment and Follow-Up Care
Treatment depends entirely on the underlying cause.
- Atrophic changes are typically managed with localized vaginal estrogen therapy.
- Polyps are removed through hysteroscopic polypectomy.
- Endometrial hyperplasia without atypia is treated with progestin therapy.
- Hyperplasia with atypia often requires hysterectomy due to cancer risk.
- Malignancies require referral to a gynecologic oncologist for staging and treatment.
Ongoing follow-up is essential, particularly for patients treated conservatively or those with high-risk factors
Conclusion

Bleeding occurring two years after menopause should never be ignored. While the cause may be benign, prompt medical evaluation is essential to rule out serious conditions and ensure optimal health outcomes.
Menopause is a unique journey for every woman. With timely medical guidance and expert care, you can confidently navigate this phase while prioritizing your well-being.
Whether it is seeking evaluation for post-menopausal bleeding or treatment for female infertility treatment in Mumbai, we are here to support you.
Contact us Babies & Us Fertility Center to schedule an appointment with our experienced gynecologists and IVF specialists in Mumbai for personalized and expert care.
FAQs
Q1. Is bleeding after menopause ever normal?
No. Any bleeding after menopause should be evaluated by a healthcare professional.
Q2. What are common non-cancerous causes?
Uterine or cervical polyps, vaginal atrophy, infections, and hormone therapy are common benign causes.
Q3. Can postmenopausal bleeding indicate cancer?
Yes. Conditions such as endometrial hyperplasia or cancer must be ruled out promptly.
Q4. When should I seek medical care?
Immediately, especially if bleeding is recurrent, heavy, painful, or persists for more than a few days.